The elbow is a complicated joint. In fact, it is one of the most complicated joints in the entire body. The elbow also plays an extremely important role in our day-to-day activities; so, as you can expect, problems with this joint can greatly disrupt our functioning. Naturally, elbow problems tend to underscore just how important the elbow can be. Tasks that were easy before, such as working or driving, become nearly impossible to those with elbow irritation.
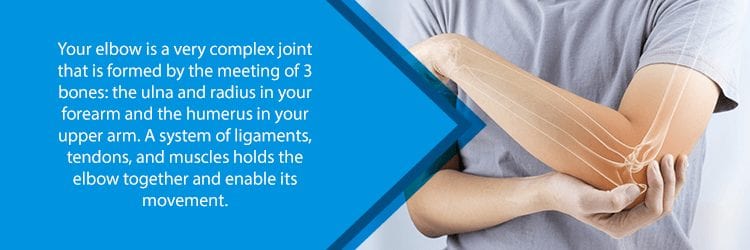
Aside from being one of the most complicated joints in the body, the elbow is also one of the largest joints as well. Specifically, the elbow connects the radius and ulna to the humerus, which are fairly large bones on their own. Furthermore, the elbow connects these parts through a system of ligaments and muscles. Precisely because of the elbow’s size, complexity, and location, it can alter our range of motion immensely.
Not only is the elbow very large and complicated, but it is also one of the most frequently used and abused joints in the human body. Inherently, this means that the elbow is prone to injuries, such as fractures and hyperextension. For example, there are many orthopedic conditions associated with the elbow, such as bursitis and osteoarthritis. NJ Spine and Ortho can help you understand your symptoms and seek treatment.
Arthroscopic Surgery For Elbow Bursitis
Elbow bursitis is a painful condition that involves inflammation of the bursae. Bursae are small, fluid-filled sacs that cushion the bones, tendons, and muscles near the body’s joints. When these sacs become inflamed, doctors call the condition bursitis.
Bursitis is not necessarily exclusive to the elbow joint. It may also occur in the knee, shoulder, hip, heel, or base of the big toe. Usually, bursitis predominantly affects the elbow, shoulder, and hip, as these are the joints that undergo the greatest strain.
Not all cases of elbow bursitis require surgery. In fact, most of the time, these inflamed sacs will get better on their own. That being said, there are more severe instances in which a doctor must surgically drain the inflamed sac. In the most severe cases, it may even be necessary to remove the affected bursa altogether. This, however, is exceptionally rare.
If conservative treatments have not alleviated the patient’s symptoms, your doctor will perform surgery. Usually, bursitis surgery is performed using a small incision with a minimally invasive probe known as an arthroscope. An arthroscope is a pencil-sized device with a small lens that the surgeon inserts through an incision to receive 3D guidance. This allows the surgeon to make repairs and corrections to the joint as necessary. Another hidden benefit of elbow arthroscopy is that this surgery is minimally invasive. This means that the procedure boasts a faster recovery time than traditional open surgeries.

Minimally Invasive Surgery For Rheumatoid Arthritis (RA)
RA is one of the most common types of elbow arthritis, but it is fundamentally different than most types of arthritis. Conventionally, arthritis affects the joints over time through age-related wear and tear, but RA is a little different. Medical experts classify RA as an autoimmune disorder because the condition confuses the immune system into attacking the body’s own tissues. Unlike wear and tear arthritis, RA is known to affect the joint linings, which causes painful swelling. Additionally, this may result in joint abnormalities and bone erosion.
It is not uncommon for RA to affect multiple joints across multiple systems all over the body. RA is not just limited to joints, as it may also irritate the eyes, skin, lungs, heart, and even blood vessels. RA-associated inflammation is what leads to the condition’s potential to spread to other systems in the body. Thankfully, new types of medications and treatment options have made the prognosis for the disease much better.
If nonsurgical treatments (such as physical therapy) fail to alleviate your symptoms or slow RA progression, then your doctor may consider surgery. Surgery often helps RA patients, making their symptoms much more bearable. Additionally, RA surgery may even restore the patient’s ability to use their joints normally.

RA surgeries include:
- Synovectomy: Doctors perform a synovectomy to remove inflamed joint linings (known as synovium)
- Tendon Repair: RA sometimes causes tendons to loosen or rupture. Sometimes, this condition is repairable via arthroscopy.
- Joint Fusion: If replacement is not an option, a doctor may perform this procedure to stabilize the joint and provide the patient with relief
- Total Joint Replacement: The surgeon removes the affected areas of the joint and replaces them with a prosthetic.
Elbow Surgery For Tennis Elbow
Lateral epicondylitis, otherwise known as tennis elbow, occurs when the tendons in the elbow become overworked. Usually, this happens through repetitive motions of the wrist and arm. The condition is painful and, unlike the name suggests, is not exclusive to athletes. Any job that features repetitive motions, such as plumbing or carpentry, may cause the condition.
Normally, tennis elbow pain originates where the tendons of the forearm muscles attach to the bony bump on the elbow’s exterior. Although this is where the pain typically originates, it may also spread out into the forearm and wrist. Tennis elbow patients often describe the pain as “radiating.” People with tennis elbow tend to have a hard time shaking hands, turning doorknobs, or grasping objects.
Tennis elbow may be treated conservatively, but sometimes surgical treatments are necessary for certain cases. Surgical procedures that your doctor may use to treat tennis elbow are as follows:
- Injections: Some doctors inject botox into tennis elbow tendons. Additionally, your doctor may inject an irritant such as dextrose into the joint to relieve pain and inflammation. This is known as prolotherapy. Your doctor may also use a technique known as dry needling. This simply involves piercing the affected tendon in a variety of different places.
- Ultrasonic Tenotomy: The doctor uses ultrasound guidance to insert a specialized needle through the skin and into the target area. Ultrasonic energy vibrates the needle at a very rapid pace. It is so rapid, in fact, that it liquefies the damaged tissue, which the doctor then sucks out through a suction.
Elbow Arthroscopy for Golfer’s Elbow
Golfer’s elbow is very similar to tennis elbow. In fact, it’s pretty much exactly the same, save for one fact. Whereas tennis elbow occurs on the outside of the elbow, golfer’s elbow originates at the inside. This is where the pain occurs. Like tennis elbow, the pain may also spread into the forearm and wrist. Again, like tennis elbow, golfer’s elbow is not limited to athletes. Anyone with a job that requires repetitive elbow motions could develop the condition. The surgical procedures for this condition are pretty much the same as the ones that doctors use to treat tennis elbow.
Surgical Debridement for Osteochondritis Dissecans (OD)
OD occurs when the bone beneath the cartilage of a joint dies because of a lack of blood supply. When this happens, the bone and cartilage may break away, leading to pain and decreased motion and strength.
Most commonly, OD occurs in children and teenagers. The condition usually affects the knee, but it can also occur in the ankles and elbows, as well as other areas. Symptoms of OD usually appear after a joint injury or several months of high-impact activities. There are different levels of OD and they all depend on the size of the injury. Additionally, medical experts must consider the nature of the fragment. This includes whether the fragment detaches partially, wholly, or remains in place.
For young children, OD may heal all by itself as the bones are still growing and maturing. Other cases, however, will require surgery. OD usually necessitates surgery when there is a loose fragment in the joint. Additionally, your doctor may consider surgery if your OD is still present and your bones have stopped growing. In other cases, your doctor may consider surgery if conservative treatments have not worked for you over a period of 6-12 months. The type of surgery will depend entirely on your case, so talk with your doctor for more information.
If you have any of the conditions listed above, or simply live with chronic pain, please contact us at (855) 586-2615. You can also schedule your phone call online through our website. Our orthopedic surgeons and medical staff offer the latest in minimally invasive surgical techniques. They will work tirelessly to ensure that you receive a treatment plan that serves your specific needs.