What is a Malignant Spinal Tumor?
A malignant spinal tumor occurs when an abnormal growth of the spine spreads to nearby tissues, organ systems, or parts of the body.
When a non-spreading or “benign” tumor becomes malignant, doctors upgrade the status of the tumor to “cancerous.” Although cancers of the spine are rare, slightly less than 1% of patients will still develop a cancer of the spine. For these patients, what starts out as simple neck or back pain can morph into more severe or debilitating symptoms. If you have been diagnosed with a spinal tumor, then you may experience:
- Severe pain in the cervical (neck), thoracic (mid-back) or lumbar (lower back) spine
- Pain that erupts first thing in the morning or late at night
- Symptoms of pinched nerve pain, like tingling or numbness in your arms and hands
- Muscle fatigue, weakness, or loss of coordination
- Unsteadiness on your feet
- Blunted sense of touch, hot, cold, or pain
- Loss of bowel or bladder control
- Loss of reflexes or paralysis
- Fractured vertebrae
However, the location of the tumor on your spine will determine most of the symptoms that will arise.
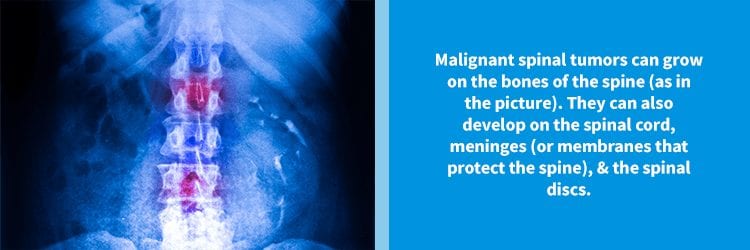
Where Do Malignant Spine Tumors Grow?
Spine cancers can develop in 3 main parts of the spine: the bones, cartilage, and discs; the meninges (or protective membranes); and the spinal cord. However, of these, Vertebral Column Tumors (VCTs) are the most common.
Your vertebral column is simply a fancy phrase for the bones of your spine. Because your vertebrae are the most exposed part of your spine, your spinal column is more prone to developing secondary tumors. Secondary means that the growth itself did not begin in your spine. For example, in women, cancers of the breast often “metastasize,” or spread, to the thoracic spine.
However, children and young adults can develop primary VCTs, which do begin in the vertebrae. (Most of the malignant tumors that we will discuss shortly are of this variety.)
Doctors classify other types of spinal tumors as Intramedullary Tumors (ITMs) if they grow within the matter, or medulla, of the spinal cord; or as Intradural-Extramedullary Tumors (if they grow on the dura of the spinal meninges). ITMs, like astrocytomas, arise from mutations in glial cells. Glial aptly sounds like “glue.” And, glial cells function to cement your nervous system together.
Intradural-Extramedullary Tumors often form on the sheathing of nerves, which can disrupt neurologic function. But, they tend to be benign. However, because they coil around the nerve roots like a toxic vine, doctors find them difficult to remove.
What are 5 Common Types of Malignant Spinal Tumors?
Malignant spinal tumors come in many different varieties. Nevertheless, some of the most common include:
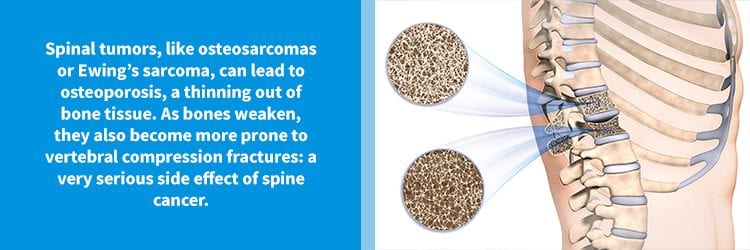
- Osteosarcoma: Also known as osteogenic sarcoma, osteosarcomas mimic the role of our osteoblasts. In a healthy spine, osteoblasts build sturdy bone to replace damaged, weak, or aging bone. However, instead, this type of tumor produces inferior bone, which weakens our skeleton as a whole. Despite this, fractured bones are rare with osteosarcomas. The most common form of all malignant spinal tumor, spinal osteosarcomas affect young adults (age 20-30) more often than all other age groups.
- Ewing’s Sarcoma: Ewing’s Sarcoma is the second most common type of spine cancer in teens, with men being marginally more affected than women. Although researchers don’t 100% understand the cause of Ewing’s Sarcoma, it is thought to result from a chromosomal mutation. Unlike osteosarcomas, this type of malignant spine tumor does lead to spine fractures. Other defining symptoms include fever and warmth to the touch at the site of the tumor.
- Chondrosarcoma: This type of VCT affects the cartilage that cushions our vertebrae, spinal discs, and facet joints. In skeletally mature adults, chondrosarcoma is the second most common type of spine cancer. It can affect any region of the adult spine, from the neck all the way down to the sacrum, and sometimes, even the pelvis. Of the 3 subtypes of chondrosarcoma, two are classed as “aggressive” or fast-growing.
- Astrocytoma: Astrocytomas arise from astrocytes, a form of glial or supportive cell. These abnormal cells can also multiply in the brain, but spinal astrocytomas wind around the nerves that exit from the spinal cord. The most aggressive form of astrocytomas are known as glioblastomas; the least aggressive are termed pilocytic. Because these tumors warp around the nerve sheath, your doctor may need to use radiation therapy to treat them.
…But What Happened to #5?
The last form of spine cancer to make our list is somewhat of a unique exception. Technically, Multiple Myeloma is not a cancer of the spine. In reality, Multiple Myeloma occurs when the plasma cells of our immune system begin to divide at uncontrolled rates. But, because plasma resides within our bone marrow, Multiple Myeloma often spreads to the bones of our spine.
In addition, Multiple Myeloma can lead to a number of spine problems, including osteoporosis or “porous” bones. Weakened bones are more likely to fracture. And, because multiple myeloma often affects the thoracic spine, a patient can develop kyphosis (or hunchback) as his or her bones degenerate from general weakness.
What Next? Getting Help for Malignant Spinal Tumors
If you have been diagnosed with a malignant spinal tumor, then you need a board-certified spine surgeon who specializes in:
- Advanced pain management techniques
- Minimally invasive tumor resection (aka tumor removal)
- Decompression procedures (like Endoscopic Foraminotomy to relieve nerve compression)
- Cutting-edge radiation & chemotherapy technologies
Needless to say, cancer treatments have come a long way in the last ten years. Innovations in radiation therapy have made it possible for doctors to treat spine cancer without resorting to surgery. And, refined surgical procedures lead to less scarring, blood loss, and pain than outdated techniques.
To get your life back from spine cancer, contact NJSO today! Our spine experts use only the latest innovations in cancer treatment to resolve your pain!

