People often refer to spinal discs as the “shock absorbers” of the spine. This makes a lot of sense because these discs are essentially sponge-like partitions that are wedged between each vertebra of the spine.
As we all know, mechanical systems with a lot of moving parts tend to wear down over time. Not only does the spine move often, but our vertebrae are also not very good at handling how we use and abuse them. So, for a variety of reasons, our spinal discs may develop problems. They may wobble left, pop out right, slip here, bulge there… In short, there is a lot of potential for things to go wrong.
Luckily, there are almost as many solutions as there are problems in regards to spinal conditions. To specify a bit, discs are the most common culprits of grating back pain and stagnant neck misery. One common treatment that doctors use to treat worn-out or slipped discs is an artificial disc replacement. The main goals of this surgery are to relieve negative symptoms and achieve greater mobility in the affected area. Additionally, this procedure is minimally invasive, so there is much less collateral damage than we would see with traditional or open surgeries.

Types of Artificial Discs
Fundamentally, an artificial disc is a prosthetic device that doctors implant into the spine in order to replace an existing disc. The goal of this procedure is the elimination of symptoms and a return to normal functionality.
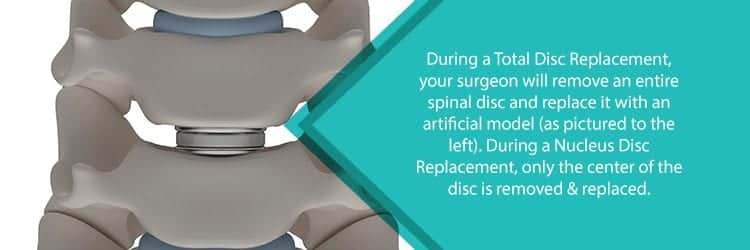
There are many different types of artificial discs, but medical experts generally classify them into two groups: total disc replacements & nucleus disc replacements. The names here pretty much give away everything you need to know about these surgeries, but the breakdown is as follows:
- Total Disc Replacement: The artificial disc used in this procedure replaces most or all of the affected disc tissue.
- Nucleus Disc Replacement: These type of devices only replace the center of the affected disc (known as the disc nucleus or nucleus pulposus). Your doctor will leave the outer ring (or annulus) intact.
Generally, metals and/or plastic biopolymer materials compose the makeup of these devices. Most commonly, total disc replacement devices have a two-plate design. In this design, one plate attaches to the vertebrae above the affected disc. The second plate attaches to the vertebrae below, effectively creating a plate-disc sandwich. Additionally, many of these devices are somewhat compressible, allowing for greater mobility. The biggest distinction from disc replacement and spinal fusion (another common procedure) is their intention. The former allows for greater mobility, while the latter eliminates it.
Nucleus replacement discs are usually made of the biopolymer material mentioned earlier. This includes materials such as hydrogel, which expands via osmosis. As previously stated, the nucleus disc replaces only the center (nucleus pulposus) of the disc. Surgeons use such expandable materials to fill the central cavity created during the procedure. Like total replacement devices, nucleus replacements are often compressible. Again, this allows for greater mobility.
Don’t worry too much though, your doctor will know the best device class to use for your condition. Just be sure to ask questions and communicate clearly and frequently.
Mobi-C Devices for Cervical Disc Replacement
We have discussed general classifications of replacement devices, so let’s get a bit more specific. The Mobi-C is a cervical disc replacement device and falls under the total replacement classification. A French doctor initially implanted this device in 2004, and the FDA approved it for widespread use in the US as of 2013.
Three parts compose the Mobi-C disc: there are two metal plates with a plastic insert in between. Generally, the plates are made up of several different metals (such as cobalt, chromium, etc.) that you will see in other spinal procedures. To help with adhesion to both vertebrae adjacent to the affected disc, the device uses small teeth. This presses the prosthetic against the vertebrae and prevents it from slipping. Most often, a coating of hydroxyapatite is applied to the plates. This coating promotes vertebral growth and improves the stability of the bond between the plates and bones.
The plastic in this device is most often made of polyethylene. Generally, this insert is round on the top, flat on the bottom, and compressible. The inventor of the Mobi-C designed all of these properties to allow for greater mobility in the patient.
The device is easy to insert, comes pre-assembled, and requires no operative steps such as bone chiseling for access. In the vast majority of cases, the surgeon completes device insertion in a single easy step.
Who Is a Good Candidate for Artificial Disc Replacement?
If you are a peruser of articles like these, chances are you have seen this before: it depends on the case. In order to determine whether or not a patient is a viable candidate for this procedure, the doctor will perform tests. These tests may include:
- Discography: An x-ray imaging technique that utilizes x-ray dyes to produce results. Your doctor injects the dye into the discs of the spine, which will reveal any tears in the disc lining.
- Magnetic Resonance Imaging (MRI): A large machine uses magnetic fields and radio waves to produce detailed images of organs and tissues.
- Computed Tomography (CT Scan): Uses a narrow x-ray beam to produce detailed images of specific bodily structures.
- X-Ray Imaging: Uses electromagnetic waves to produce images of the body’s internals.
These are just a few of the most common tests. Your doctor will decide which test to use based on the information that you give him/her about your condition.

Not all patients need artificial disc replacements. More commonly, doctors will opt for more conservative options before considering any surgery. However, people who need disc replacements generally share the following traits:
- The patient has an annular tear, bulging disc, collapsed disc, or slipped disc
- The patient has been diagnosed with degenerative disc disease
- Chronic back pain that conservative methods cannot alleviate
- No spinal deformity is present
- No prior major spinal surgeries have taken place
- The patient is not excessively overweight
These are just a few examples that determine a patient’s candidacy for artificial disc replacement. Your doctor will be able to give you more information about your specific case. In addition, there are also instances where an artificial disc replacement is not a viable treatment option. These cases involve patients with the following conditions:
- Spondylolisthesis (a slipped vertebra)
- Osteoporosis (weak or porous bones that fracture easily)
- Spinal tumor
Artificial Disc Replacement Procedure
As previously mentioned, this procedure does not involve many steps. That said, it still may take your doctor 2 to 3 hours to perform a disc replacement.
First, the surgeon will choose the angle from which he or she would like to access the spine. This will depend on which region of the spine is affected. The surgeon will then make a small incision near the affected area. Next, the surgeon will move blood vessels and other tissues to the side to avoid any unnecessary collateral damage. In addition, this step allows for better access to the spine without the added difficulty of moving nerves. Once the surgeon is able to access the disc, he or she will either entirely remove it or remove just the center. The surgeon then replaces the disc with the artificial device and closes the incision.
Usually, the recovery period for this procedure is 1 to 3 days. However, the length of this period will vary depending on the patient’s level of pain and functionality.
If you have any pain-related back complaints, please contact us at (855) 586-2615. NJSO has a team of highly-trained back surgeons in NJ who are well-versed in minimally invasive surgical applications. Our doctors will make sure to find a treatment program that suits your specific needs.

