Infections occur when bacteria, viruses, or other microorganisms invade the body. Some infections clear up on their own. Unfortunately, some can cause severe or even life-threatening conditions. Compared to the common cold and flu, spinal infections are relatively rare. When someone gets a spinal infection, however, some form of treatment is often necessary.
Use this guide from NJ Spine and Ortho to understand the causes and risk factors of a spinal infection. You will also discover what treatment options are available to get your life back on track.
Understanding the Spine and Spinal Infections
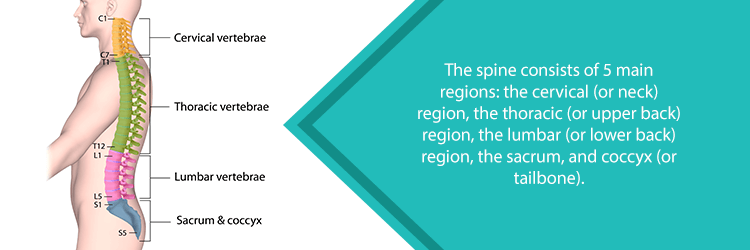
To better understand spinal infections, it helps to familiarize yourself with the spine. The spine provides support and balance to the body during movements. It also helps protect the spinal cord, nerve roots, and vital organs.
The spine consists of 33 bones called vertebrae. They interlock to form the spinal column. These bones are divided into 5 regions: the cervical (or neck) region, the thoracic (or upper back) region, the lumbar ( or lower back) region, the sacral region (located near the hips), and the coccygeal (or tailbone) region. An opening runs through the middle of these bones known as the spinal canal. The spinal canal houses the spinal cord—a bundle of nerve fibers that connects the brain with the rest of the body. In addition, the spinal cord allows the brain to communicate with the rest of the nervous system.
In between these vertebrae are circular discs. These intervertebral discs help to protect the bones of the spine by absorbing the shock of movement.
How the Spine Becomes Infected
A spinal infection normally occurs when a bacterial, viral, or fungal infection from another area of the body reaches the spine. Staphylococcus aureus, a bacterium known for causing several illnesses like pneumonia and strep throat, is the most common pathogen to cause spinal infections. In fact, the methicillin-resistant strain of this bacterium, known as MRSA can account for up to 60 percent of spinal infections.
Another bacterium found in the body’s natural flora, Staphylococcus epidermidis, has found to be the cause of spinal infections for those who recently received implants or pacemakers.
Types of Spinal Infections
Infections are typically known by the area of the spine they affect. These include:
- Vertebral Osteomyelitis: The most common spinal infection, which usually affects the lower back region of the spine. This infection attacks the bones of the spine, known as vertebrae.
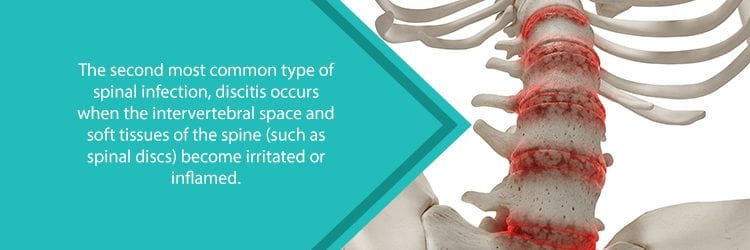
- Discitis: Inflammation in the intervertebral disc space. Swelling in this area may put pressure on the discs, which in turn leads to pain. This can also cause swelling in the surrounding joints and soft tissues.
- Meningitis: An inflammation of delicate membranes which cover the brain and spinal cord. Viral meningitis is usually resolved without treatment. Bacterial meningitis can be contagious and even life-threatening.
- Spinal Epidural Abscess: An infection that develops in the space around the soft tissues which surround the spinal cord and nerve roots. The body uses white blood cells to fight the infection which causes pus to build up and create an abscess. Pus is a collection of immune cells, dead cells, and lingering bacteria.
- Spinal Cord Abscess: This rare condition is often a complication of a spinal epidural abscess. As the abscess grows, it puts pressure on the spinal cord, known as spinal stenosis. This causes very serious symptoms like paralysis and a loss of sensation below the abscess.
Who is at Risk for Spinal Infections?
Anyone can develop a spinal infection. Here are some common risk factors:
- A history of intravenous drug use
- Being over the age of 50
- Having undergone a recent surgery
- Tobacco use
- Human Immunodeficiency Virus (HIV)
- Malnutrition
- Diabetes
- Arthritis
- Previous organ transplant
- Cancer
- Recent history of a urological procedure
- Previous procedure using a vascular device
- Back injuries or trauma
- Overweight or obese
- Long-term use of steroids
Symptoms of Spinal Infections
The symptoms of spinal infections tend to vary. Some may not even feel any symptoms until days or weeks after the initial infection. The most common symptom is neck and back pain, which is not caused by a known injury or trauma. Some people also develop a fever.
Symptoms of the most common spinal infection, vertebral osteomyelitis, can also include nausea, fatigue, and irritability. In addition, there may be redness and warmth in or around the infected area. Swelling around the bone can lead to a loss of range of motion.
Other symptoms of spinal infections include:
- Weight loss
- Chills
- Pain while trying to sleep
- Worsening pain over time
- Radiculopathy or pinched nerves
- Difficulty controlling the bladder or bowels
- Numbing or weakness in the arms or legs
- Partial paralysis
- Swelling at the infection site
- Deterioration of the vertebral body
Diagnosing a Spinal Infection
Symptoms of a spinal infection can mimic other neck and back conditions. A doctor must perform a thorough exam with diagnostic imaging and laboratory tests to rule out other conditions and achieve an accurate diagnosis.
Laboratory Tests
Almost 90% of those who suffer from a spinal infection have an elevated erythrocyte sedimentation rate (ESR). The ESR detects inflammation in the body caused by infections or autoimmune diseases. The ESR is not a diagnostic test for spinal infection. Instead, it indicates that the body is currently struggling with an inflammatory condition. A ESR test involves a blood sample. The results could be ready in as little as a half hour.
Another common blood test that can help to diagnose a spinal infection is the C-reactive protein levels (CRP). CRP is a substance that the liver produces to increase inflammation in the body. This simple blood test may take a few days to return results.
Your doctor may also order a white blood cell count (WBC) test. The white blood cells play a key role in fighting infection and inflammation. An elevated level of these cells could signal a serious infection. You can get results from a WBC test in about a day.

Imaging tests
If a spinal infection is suspected, one of the most effective imaging tests is magnetic resonance imaging (MRI). Diagnosis from this test can be observed within a few days of the infection. This test uses a computer, powerful magnets, and radio waves to create detailed pictures of the inside of your body.
X-rays may also be used to detect any narrowing of the disc space or issues with the bones of the spine. Your doctor may also use a computed tomography scan (CT scan). This is a specialized X-ray that allows the doctor to view your body in sections (like how one would look at a loaf of bread after slicing it).
Other Testing
Once your doctor detects the presence of a spinal infection, your physician will typically order further bacteriological tests to determine the source of infection. This could include blood, urine, and spit cultures. This allows the doctor to select the best medicines to treat your condition.
Treatment for Spinal Infections
If your spinal infection is caused by bacteria, the first line of treatment often involves antibiotic medications. Typically, these drugs are given through the veins (i.e. intravenously) as opposed to by mouth (or orally). This allows the drugs to swiftly and effectively reach the source of your infection. Depending on your infection, antibiotic treatment can last from a week to a couple months.
During that period, you may also be prescribed a period of rest as well as spinal bracing. These braces enable you to keep your spine stable and injury-free as it heals.
In many cases, medications will clear up the infection. If antibiotics aren’t working, more aggressive treatments may be necessary. Surgical treatments are helpful when there are neurological problems, deformity, and instability to the spine or recurring infections.
If surgery is suggested, debridement of the area and bone grafting is the standard for treating your infection. A surgeon will clean and remove the infected tissue. Depending on the severity of your condition, a discectomy—removal of the infected, damaged disc—may be necessary. If this is the case, a spinal fusion procedure will add a piece of bone from another area of your body (or a bone bank) to the area where the disc was removed. This enables the two bones surrounding the removed disc to fuse together creating one bone. In many cases, doctors can perform these as minimally invasive procedures.
If you’re suffering from a spinal infection, using a multidisciplinary team of experts leads to the most effective results. Physicians, spine surgeons, infectious disease experts, and other professionals who are specifically trained in dealing with this complex condition will provide you with an individualized approach and the most appropriate treatment options.
Where Can I Get Help for My Spinal Infection?
NJ Spine & Orthopedic provides a comprehensive program for diagnosing and treating all your spine pain issues. Our experienced, dedicated team knows each patient wants to get his or her life back. This is why we use the latest proven approaches for treating pain.
From your first call to (855) 586-2615 until the end of your recovery period, NJ Spine & Orthopedic wants to make sure you are comfortable and well-informed about all your treatment options. Schedule an appointment today to take the first step toward a better life!

