Roughly 10 million Americans have osteoporosis and an additional 34 million have low bone mass. Both of these conditions increase your chances of developing a compression fracture by a considerable amount. However, this condition does not affect the genders equally, with 8 of the 10 million osteoporosis patients being women.
Vertebral compression fractures (VCF) are extremely common in patients with osteoporosis, affecting around 750,000 people every year. In postmenopausal women, VCFs affect about one-fourth of this group. The incidence and prevalence of VCFs naturally increase as patients age. In fact, a staggering 40% of women age 80 and older will suffer compression fractures. While the condition may be far more common in women, it nevertheless constitutes a major health issue for older men as well.
A VCF describes a type of fracture or breaks in the vertebrae. Vertebrae are the bones in your back that stack up, one on top of the other, to make up the spine. Your spine has a large number of functions: it supports your weight, allows you to move, and protects vital components of your nervous system. Compression fractures cause the vertebrae of the spine to collapse, which in turn makes them shorter. When these collapses occur, pieces of bone may press on the spinal cord and nerves, decreasing the amount of oxygen and blood flow that the spinal cord would normally get.
In most cases, these fractures heal with medications, bracing, and rest. With time, most people are able to return to their everyday activities. Some cases, however, are more serious and may require surgical treatment.
Causes of Vertebral Compression Fractures (VCFs)
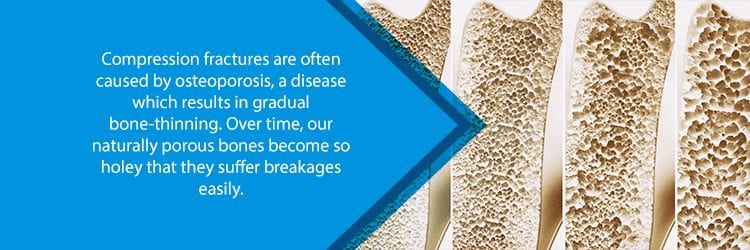
At the heart of the problem always lies softer, weakened bones. Generally speaking, compression fractures usually occur because of the bone-thinning condition known as osteoporosis. This is especially true for women over the age of 50 who have been through menopause.
When your bones are more brittle than they should be, your vertebrae, in turn, are not strong enough to support your spine throughout the activities that you perform every single day. This includes simple actions, such as lifting objects, missing steps, slipping on the carpet—all of these things increase your risk of a VCF. Even the most minor coughing or sneezing spells may result in compression fractures if you have osteoporosis.
After your body has undergone numerous small VCFs, you will begin to show all manner of symptoms. Your spine becomes shorter due to the loss of height in the vertebrae, and the strength and shape of your spine become subject to change.
Most of these fractures occur in the frontal region of the vertebrae. If this happens often enough, then the affected vertebrae will eventually collapse. The front of the vertebrae is often more affected than the back because it is made up of harder bone, making it more difficult to crack. Because of this, VCFs create wedge-shaped vertebrae, which leads to a stooped posture that many people refer to as dowager’s hump. Your doctor or other medical professionals may refer to this symptom as kyphosis.

Risk Factors for VCFs
As mentioned, one of the biggest risk factors for VCFs are bone diseases such as osteoporosis. That being said, patients with cancer that has spread to the bones may also find themselves at the mercy of VCFs. If you have certain types of cancer—such as lymphoma or multiple myeloma—keep an eye out for compression fractures. In fact, sometimes a spinal fracture is one of the first signs of cancer.
But again, most VCFs happen because of osteoporosis. However, some patients have a higher chance of developing this disease over others, because of:
- Race: White and Asian women are at a much greater risk of developing osteoporosis.
- Weight: Women who are thinner than average are also at a much greater risk for developing the condition.
- Age: The chances of developing osteoporosis become much higher as the patient advances in age.
- Gender: In general, women are much more likely to develop osteoporosis than men are.
- Smokers: Smokers tend to lose bone thickness much faster than those who do not smoke.
- Early Menopause: Women who go through menopause before the age of 50 are at a much greater risk of developing this condition.
You may have osteoporosis and not even be aware of it. As a matter of fact, around 66% of VCFs are never even diagnosed as many people mistake them as natural aging pains or arthritis. If the condition is not treated, however, your health may exacerbate over time as you develop more fractures. If you have back pain, then you should consider seeing a doctor just to be on the safe side.
Symptoms of Vertebral Compression Fractures (VCFs)
When compression fractures first start, they may not manifest symptoms. Your doctor may be able to discover them on an x-ray while looking for something else entirely different. That being said, in later stages symptoms may include:
- Back pain that worsens with time. Patients claim that lying on your back tends to make the pain lessen while standing up makes it worse.
- A decrease in overall height.
- The movement of the spine becomes more limited. For example, you may have trouble bending or twisting.
- Patients may take on a stooped-over posture known as kyphosis. This occurs because the front part of the vertebra is generally the part that loses height, leading to the front-leaning posture.
- Numbness or tingling, weak muscles, difficulty walking, and loss of bowel/bladder control may also occur.
- In cases where the fracture happens quickly, you may feel sudden, severe back pain.

How are Vertebral Compression Fractures (VCFs) Treated?
If you have VCFs due to osteoporosis, then your doctor will use treatments for that condition. Naturally, your doctor may recommend that you take bone-strengthening medicine as well as calcium and vitamin D supplements. He or she may also share with you vital physical therapy exercises to help alleviate your pain. All of these things work together to make your bones stronger and prevent future VCFs.
Other forms of treatment may include:
- Pain medication to relieve uncomfortable sensations
- Periods of rest to allow for your bones to heal—this includes limiting activities
- Wearing a back brace for a period of time
- Using physical therapy to help you expand your range of motion and also to strengthen the bones that surround the spine
Most cases do not require the need for surgery, but there are definitely scenarios in which it is applicable. If the above treatments do not help, your doctor may recommend these commonly used procedures:
- Vertebroplasty: Throughout the procedure, your performing surgeon will use x-ray guidance to maneuver around the relevant regions of your spine. The basic gist of this procedure involves using a small needle to inject a specialized quick-setting cement into the affected vertebrae. This material will provide support for the broken vertebrae, and usually, it results in pain relief for the patient.
- Kyphoplasty: This procedure is very similar to the last, except there is the addition of small balloons which your surgeon will use to expand the fracture space. Naturally, this helps make your vertebrae taller. Once this occurs, your surgeon will then remove the balloons and fill the affected area with the specialized cement.
Contact Us
Do you have back pain that doesn’t seem like it is going to get better anytime soon? If so, please contact NJ Spine and Orthopedic at (855) 586-2615. Our staff is filled with medically trained experts who are well-versed in the art of pain management and minimally invasive surgical procedures. We will work tirelessly to ensure that you are put on a care plan that suits your specific needs. Contact us today!

