Common symptoms, such as lower back and leg pain, can have several causes. In many cases, these pain indicators signal a muscle sprain or an injury to our connective tissue. In fact, some back pain simply goes away on its own with rest and conservative treatments. Ice/heat therapy or anti-inflammatory medications may be all that you need.
For some, the causes of back pain are more serious. A herniated or slipped disc, arthritis, or an injured nerve can cause significant pain that doesn’t fade away on its own. These conditions usually require the help of a doctor or orthopedic surgeon to achieve pain relief.
In some cases, damage to the nerves or nerve roots is a medical emergency that requires immediate attention. This is especially true for those who suffer from cauda equina syndrome (or CES). When your back pain includes weakness or numbness in the legs and/or bladder and bowel dysfunction, you should seek immediate care to prevent permanent damage.
The Spinal Cord & Cauda Equina
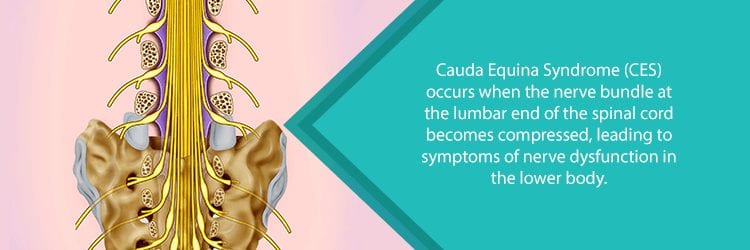
As you may know, the spinal cord is the passageway where messages are sent to and from the brain. Running through your spinal column, the spinal cord is responsible for relaying messages involving movement, organ function, and sensory input—among many other things. Damage to the spinal cord significantly impacts the way in which your body functions.
At the bottom of your spinal cord is a bundle of nerve roots known as cauda equina. The name comes from a Latin phrase meaning “horse’s tail”. This is because these nerve roots begin at the base of the spinal cord and branch out to the lower body resembling, well, a horse’s tail. These nerve roots are responsible for sending and receiving messages from the lower limbs. In addition, they play a key role in controlling the pelvic organs like the bladder and bowels.
Compressed nerve roots disrupt the function of the legs and pelvic organs. Without treatment, a compressed cauda equina can lead to permanent paralysis and chronic incontinence. It may also result in sexual dysfunction.
Causes & Symptoms of Cauda Equina Syndrome (CES)
One may experience a quick onset of CES symptoms or they can develop over time. This depends on what is actually causing the nerves to compress. The following are common causes of CES:
- Lumbar Herniated Disc: The gel-like discs between each vertebra can become damaged by falls, sports injuries, or car accidents. Also, as we age our discs slowly begin to lose shape and structure which can compress the nerve roots.
- Spinal Fracture: Traumas and injuries can also cause damage to the structure of the spinal column, leading to fractures. In addition, conditions like osteoporosis may put the spine at a greater risk for fractures.
- Lumbar Spinal Stenosis: Narrowing of the spinal canal—which houses the spinal cord. Older adults may gradually develop this condition because of changes in spinal structure.
- Spinal Tumor: A growth occurring on or near the spinal cord can compress nerves. Tumors may or may not be cancerous.
- Spinal Infection: Bacterial or fungal infections may reach the spine or intervertebral discs through the bloodstream. The resultant inflammation can compress nerves and nerve roots.
- Failed Back Surgery: While back surgery can help many people relieve pain and regain function, sometimes it is not successful. Recurrent back problems or scar tissue around the nerve root can lead to cauda equina syndrome.
- Arteriovenous Malformation (AVM): An abnormal tangle of blood vessels on or near the spinal cord. This disrupts blood flow causing spinal tissues to deteriorate or die. Most AVMs are present at birth.

Symptoms of Cauda Equina Syndrome (CES)
The cause of your cauda equina compression will determine how quickly your symptoms develop. Some experience a quick development of symptoms—in as little as 24 hours. Others may feel symptoms come and go, progressively becoming worse over time. Common symptoms of CES include:
- Saddle Anesthesia: Areas of the groin, genitals, buttocks, and inner thighs experience weakness, numbness, or tingling.
- Neurogenic Pain: In addition to the “saddle” region, you may experience numbness or weakness in the legs and feet. It may present on one side (unilateral pain) or both sides (bilateral pain). This causes difficulty walking or standing.
- Incontinence: Bladder or bowel dysfunction is a major “red flag” for this syndrome. This includes lack of sensation while urinating, urinary retention, or loss of rectal control.
- Lower Back & Leg Pain: Although this symptom can be caused by many conditions, when accompanied by the above symptoms, you should seek medical help immediately.
Diagnosing & Treating Cauda Equina Syndrome (CES)
Properly diagnosing CES poses some difficulties because the symptoms are similar to other lower back conditions. For example, a herniated disc and peripheral nerve disorder share some of the exact same symptoms. If you do experience incontinence or saddle anesthesia, however, this could raise a “red flag” for CES.
In addition to receiving a physical exam, doctors generally use magnetic resonance imaging (MRI) to take a better look at the cauda equina area. In some cases, a special X-ray of the spinal canal—known as a myelogram—can help with diagnosis. Remember, the quicker you get a positive CES diagnosis, the more likely you will be to avoid permanent nerve damage and lingering issues.
Treatments for Cauda Equina Syndrome (CES)
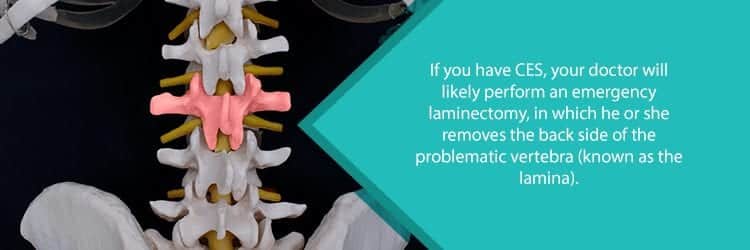
Prompt surgical interventions are usually needed for CES—especially with a sudden onset of symptoms. In fact, those who receive surgical decompression of the cauda equina nerves within 48 hours of symptom onset have the best chance at achieving a successful recovery.
In many cases, a surgeon will perform a lumbar laminectomy on the affected nerves. Depending on your condition, this can be an open or a minimally invasive surgery. During surgery, the source of compression is found and then removed. This can include removing bone spurs and portions of the laminae—part of the vertebral arches forming the top of the spinal canal.
If a herniated disc causes the nerve compression, then the surgeon may elect to do a microdiscectomy. This procedure removes part of a herniated disc so that it no longer presses on the nerves. Depending on how much of the disc is removed, spinal fusion or special hardware may be required to keep the spine stable.
For those with spinal tumors, chemotherapy or radiation therapy may be necessary after the nerves are decompressed. This helps to reduce the size of tumors.
Recovery from CES Surgery
As mentioned above, receiving surgery as soon as possible plays a major role in your recovery. The less the nerve damage, the more likely you will be able to regain all or most of your functioning. Right after surgery, you may still experience issues with pain, bladder and bowel dysfunction, and muscle weakness. In some cases, depending on the extent of nerve damage, you may be able to once again enjoy a normal life.
Physical or occupational therapy may be helpful in addressing these symptoms and regaining function in your legs, bladder, or bowels. Some people also find emotional support helpful in dealing with the painful, sometimes embarrassing, symptoms following a CES surgery. This is especially true if these symptoms become chronic.
Don’t Delay Getting Help for Cauda Equina Syndrome (CES)
Time is crucial if you notice the “red flag” symptoms of CES. Not taking the extra time to search for a qualified orthopedic surgeon can put you in serious risk for permanent, debilitating damages. NJ Spine & Orthopedic is ready to help. We understand the importance of a quick and effective surgical intervention for CES. And, rest assured, our doctors have decades of experience in treating spinal conditions like cauda equina syndrome.
NJ Spine & Orthopedic uses the latest medical technology and approaches for finer precision and less postoperative pain. Don’t delay—even if you aren’t sure you’re suffering from CES. It’s better to be safe than sorry.
Calling (855) 586-2615 today puts you in touch with a dedicated team ready to treat your CES and minimize the potential for permanent damage.

