Pain affects the quality of our day-to-day lives. Even life’s simplest pleasures can be difficult to enjoy if you suffer from chronic pain. You may not be aware of the source, but injured or neglected muscles can be the cause. By finding the root of your pain, you can regain control of your life.
This may involve taking a look at muscles that you never even knew existed, such as the piriformis muscle.
If pain in the buttocks, legs, and lower back has you sidelined from doing the things you love, it’s time to find the cause. NJ Spine & Ortho is here to help.
Understanding Piriformis Syndrome
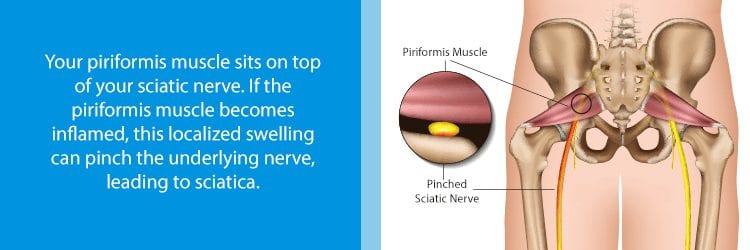
When a small muscle deep in the buttocks gets injured, it can put pressure on the sciatic nerve. This pressure causes tingling, numbness, and shooting pain. To better understand piriformis syndrome, let’s take a look at the body parts to blame for this condition.
Your Piriformis Muscle
Chances are you’ve never even heard of this muscle unless you’ve injured it. The piriformis muscle is located behind the gluteal muscles of the buttocks. This pyramid-shaped muscle runs from the sacrum (base of the spine) all the way to the top of the femur (or thigh bone).
The piriformis muscle helps the leg and foot to rotate outward. In addition, it provides stability while standing, walking, and engaging in other leg movements.
Your Sciatic Nerve
The sciatic nerve is the largest nerve in the body. It starts at the lower spine and stretches from the buttocks through the thighs. It then branches out carrying signals all the way down to the feet.
The sciatic nerve lies very close to (and can even pierce) the muscle fibers of the piriformis. Since our bodies are different, the relationship between the piriformis muscle and sciatic nerve will vary. Less than 15% of cases occur due to a person’s anatomy. But, when this happens, the condition is known as primary piriformis syndrome.
More likely, the condition will emerge due to trauma or poor personal habits. When the piriformis muscle gets injured or inflamed, it puts added stress on the sciatic nerve. As a result, one may start to feel the symptoms of secondary piriformis syndrome in action.
Piriformis Syndrome Symptoms
Symptoms of piriformis syndrome can occur suddenly when injury or trauma are involved. In other cases, symptoms will slowly worsen or disappear and then re-emerge over time. In fact, one of the most common signs of piriformis syndrome is feeling buttock or upper leg pain after sitting for over twenty minutes.
Other symptoms include:
- Tingling or numbness in the buttocks or upper legs
- Tenderness in the butt muscles
- Radiating pain from the buttocks down the leg, stopping just short of the knee
- Less range of motion in the hip joint
- Pain after long periods of lying or standing
- Shooting pain when rising from a chair
- Brief pain relief after walking
- Pain during bowel movements
You may confuse piriformis syndrome with other conditions such as sciatica, lower back pain, or issues with the hamstring. In fact, some of these problems share very similar features. This is why it is crucial to consult with a doctor when you experience these symptoms. Proper diagnosis is key to your recovery.
What are the Risk Factors for Piriformis Syndrome?

Anyone can develop piriformis syndrome. However, it is more common in middle-aged people. In addition, women are more likely to suffer from this condition than are men. This may be due to differences in female vs. male anatomy. Other risk factors include:
- Injuring the buttocks during a car accident or fall
- An inactive lifestyle with long periods of sitting
- An abrupt change in exercise or activity habits
- Increased muscle tension due to excess stomach weight (i.e. pregnancy, obesity)
- Repetitive exercise or movements, such as running
- Improper stretching before or after vigorous exercise
Diagnosing Piriformis Syndrome
There are no specific tests to diagnose this condition. Doctors often begin by reviewing a patient’s complaints and medical history. This helps to rule out other conditions such as a herniated disc. Since some doctors base their diagnosis solely on reported symptoms, piriformis syndrome can be easy to misdiagnose.
An experienced clinician, however, will use a complete medical history and exams to assess a patient. These tests may include:
- X-Rays: Although an X-ray won’t be able to detect piriformis syndrome, it can rule out other conditions like compression fractures, bulging discs, or spinal stenosis.
- Magnetic Resonance Neurography (MRI): This type of imaging allows your doctor to see just how the piriformis muscle affects the sciatic nerve.
- Complete Physical Evaluation: Doctors or even physical therapists may complete an exam to assess your physical condition. During this eval, your doctor will check your pelvis, hip joints, sacrum, and lumbar spine.
- FAIR Test: One especially effective exam involves testing the flexion, adduction, and internal rotation of the hips. These movements can cause the piriformis muscle to stretch, resulting in compression of the sciatic nerve.
Treatment for Piriformis Syndrome
Early diagnosis and treatment of piriformis syndrome is the best way to achieve a full recovery. In mild cases, self-care can allow the issue resolve on its own. Stretches, rest, and applying heat and cold to the affected area can all speed up the recovery process.
In severe cases, more aggressive tactics may help. Doctors often prescribe these therapies when self-management doesn’t work. Advanced treatments may include:
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDS) can help to reduce the pain and inflammation of the piriformis muscle. Those using NSAIDs often report a reduction in symptoms within a week.
Doctors may also prescribe muscle relaxants and pain medications for those who suffer from severe pain. Due to the nature of these addicting drugs, you should only use these as prescribed. For those with a history of substance abuse, other alternatives may be necessary.
For more stubborn cases, doctors may inject medicine directly into the affected area. These injections use steroidal medications to help reduce soreness.
Massage
Massage is also a great way to manage your pain and speed up your muscle recovery. You could perform some self-massages or recruit the help of a massage therapist (MT). Trained MT’s can identify trigger points and use pressure to release these knots. Massage also helps to improve blood flow and reduce pain.
Physical Therapy
A PT, chiropractor, or doctor can also prescribe sets of stretching and strengthening exercises. These movements increase the strength and range of motion of the nearby muscles and joints. Typically, these exercises are demonstrated and practiced in a professional setting. Once the patient gains confidence, he or she will perform short sets of these exercises at home.
Examples of Common Exercises used to Treat Piriformis Syndrome:

Listed below you will find a series of exercises that are often used to speed up the healing process. If your condition causes severe pain, then speak with a professional before trying these out at home.
- Side Lying Hip Abduction: Lay on your side with your bottom leg bent at about a 45-degree angle. Keeping your upper leg straight, lift it slowly. Then, return to your starting position. Repeat this exercise 15 times or as tolerated. Then, turn to your other side and raise the other leg.
- Side Kick: Start in a position similar to the above. Your lower leg should be bent and you upper leg held out straight. In a smooth, controlled movement, kick your upper leg forward. Slowly return to your starting position. Repeat this exercise as tolerated and then switch sides.
- Clamshells: Lay on your side with both legs bent at about a 45-degree angle. Keeping your upper leg bent and feet together, raise it at the knee. This exercise will have your legs looking like a clamshell opening its mouth. Bring your legs back to your starting position and then repeat. Turn over to your other side and repeat the movement.
Surgery
When other treatment options fail, you may wish to consider surgery as a last resort. A minimally invasive procedure can help to reduce muscle tension on the piriformis. In addition, your doctor may insert a tiny scope to explore the SI joint or sciatic notch. This will aid your doctor in determining just how your muscle fibers may interact with your sciatic nerve. Though this is a more aggressive approach, the overall benefits may be worth it.
Preventing Piriformis Syndrome
We’ve listed some tips below to help you avoid the flare-ups of piriformis syndrome:
- Make sure that you warm up well before exercising.
- Stay active by walking often or engaging in other low impact exercises.
- Routinely perform exercises that strengthen the hip abductors.
- Avoid strenuous activities that cause you pain.
- Consider yoga or pilates to increase flexibility, range of motion, and posture.
- Rest any sore muscles before returning to physical activity.

When All Else Fails…
If the pain of piriformis syndrome is still affecting your life after medication and physical interventions, NJ Spine & Orthopedic can help. After a thorough exam and free readings of your previous MRIs, our board certified doctors will help you decide the next steps. If surgery is the best option for your pain relief, you can trust that our surgeons will help you “Get Your Life Back!”